Designing a Core Case Module
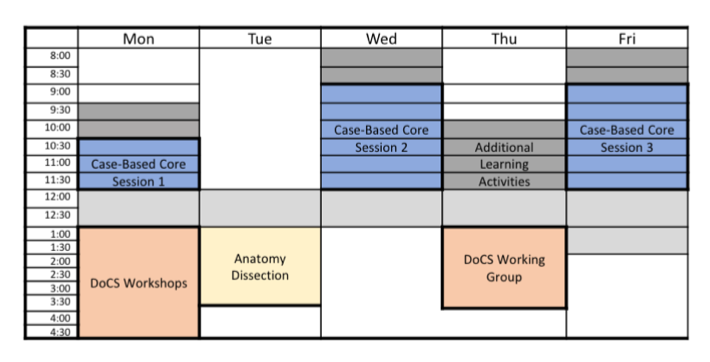
Sample Overview of a Weekly Core Case Heading link
Key terms:
- Session refers to an entire session on a given day.
- Segment refers to a part of a session.
Some clarifying information:
- Core cases can be unique to one session, two sessions, or all three in a given week.
- One example, a traveler’s medical condition case might ‘unfold’ over the course of all three sessions during that week.
- Another example, a core case on schizophrenia might take place on just one of the possible sessions during a given week, and a TBL might take one of the other possible time slots on the same or a similar topic.
- Even though 2-3 hours are allocated for a core case session, you do not have to use all of it.
Below, we have included a scenario for using the different sessions and segments.
Session 1 Heading link
- Describe case goal(s) to students and go over learning objectives. Segment 1 could consist of the HPI with or without additional information, such as family history. (This corresponds to Normal and Abnormal structures and functions).
- Provide students with task(s) and/or ask probing questions.
Examples of questions: identify risk factors, such as race, family history, and relevant review of systems pertinent to the chief complaint/case/condition. Develop a diagnostic schema (a cognitive framework for approaching a specific chief complaint).
- Segment 2 could consist of the remainder of the complete history during this same session. (This corresponds to Normal and Abnormal structures and functions).
- Provide students with task(s) and/or ask more probing questions. Examples of questions: predict physical exam findings for a few diagnoses.
Consider the underlying basic science principles and concepts contributing to the patient’s condition. Develop illness scripts among the potential diagnoses and compare/contrast them through identifying discriminating features. Identify what fits and doesn’t fit for each diagnosis.
- Segment 3 of this same session could consist of physical exam findings. (Corresponds to Normal and Abnormal structures and functions).
- Provide students with task(s) and/or ask probing questions.
Examples of probing questions: Reflect on physical exam findings to refine a few diagnoses. Consider the underlying basic science principles and concepts contributing to the patient’s condition. Develop illness scripts among the potential diagnoses and compare/contrast them through identifying discriminating features. Identify what fits and doesn’t fit for each diagnosis.
Session 2 Heading link
- Segment 4 could consist of diagnostic tests, including labs and imaging.
- Provide students with task(s) and/or ask probing questions.
Examples of probing questions: Discuss utility or positive predictive value / negative predictive value or sensitivity /specificity of studies. Would a test affect clinical decision making? Would it help the patient get better? Limit excessive testing through tiered investigation.
- Segment 5 could consist of the assessment and plan / treatment.
- Provide students with task(s) and/or ask probing questions.
Examples of probing questions: Identify potential treatments, discuss pros and cons for each. Could include differences between settings (inpatient, outpatient; ICU vs. floor).
Session 3 Heading link
- Segment 6 dives into issues related to other subthemes. (Corresponds to prognosis and practice, clinical skills – SOAP notes, simulation, oral case presentations).
- Provide students with task(s) and/or ask probing questions.
Examples of probing questions: reflect on cost of testing, false positives and negatives, and consequences, including the patient’s experience of illness, and health system issues. Discuss approach to a difficult situation (therapeutic, psychosocial, ethical, logistical challenge). Review key principles, compare courses of action.
Additional Considerations Heading link
- After each session, you should build in opportunities for students to reflect on areas of strength, as well as identify and fill gaps.
- Apply a consistent approach to clinical reasoning
Example: SNAPPS
Summarize the case including the history and findings (e.g. results of physical exam, tests, etc.) End this part with a single summary sentence. “So, in summary, this is a…”
Narrow the differential diagnosis to 2 or 3 relevant possibilities. Assuming you already know the IQ case diagnosis, consider 1 or 2 alternative diagnoses you would have considered based on the initial information you were supplied in the case (i.e. before you got the diagnosis). For example, if a baby is too large, what are the possibilities…gestational diabetes, BWS, etc. “And what I think might be going on here is…”
Analyze, then explain what information in the case was critical toward pointing you to the correct diagnosis. “The reason I was thinking of _____ (gestational diabetes) is because ______. But ____ (BWS) is also possible because the patient had _____.”
Probe – think about something related to the case you are unsure about. Make it into a question you would like to have answered by the end of your group’s case discussion. Think of something that would aid you in thinking through the case – underlying pathophysiology, basic science issue, etc. “One of the questions I have is…”
Plan – how was the patient’s problem managed or how could it be managed? “The plan being considered (or that could be considered) is…”
Select a case-related issue you would like to come back to for further learning. Ideally this would be a focused topic that you could answer in about 10-15 minutes of reading. “For me, I’d like to read about…”
- The facilitator guide should include an executive summary and answers/rationale to probing questions and tasks.